inguinal lymph nodes location
 Swollen Lymph Nodes: Locations, Causes, Signs, Test & Treatment
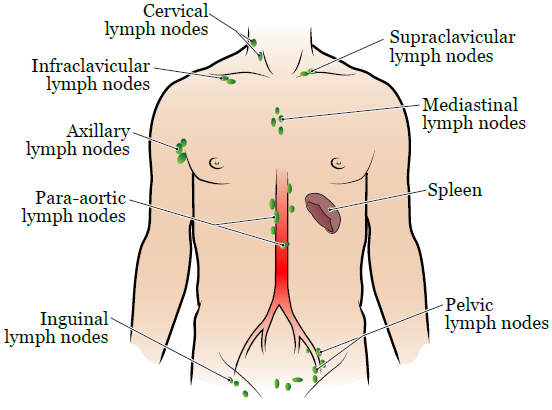
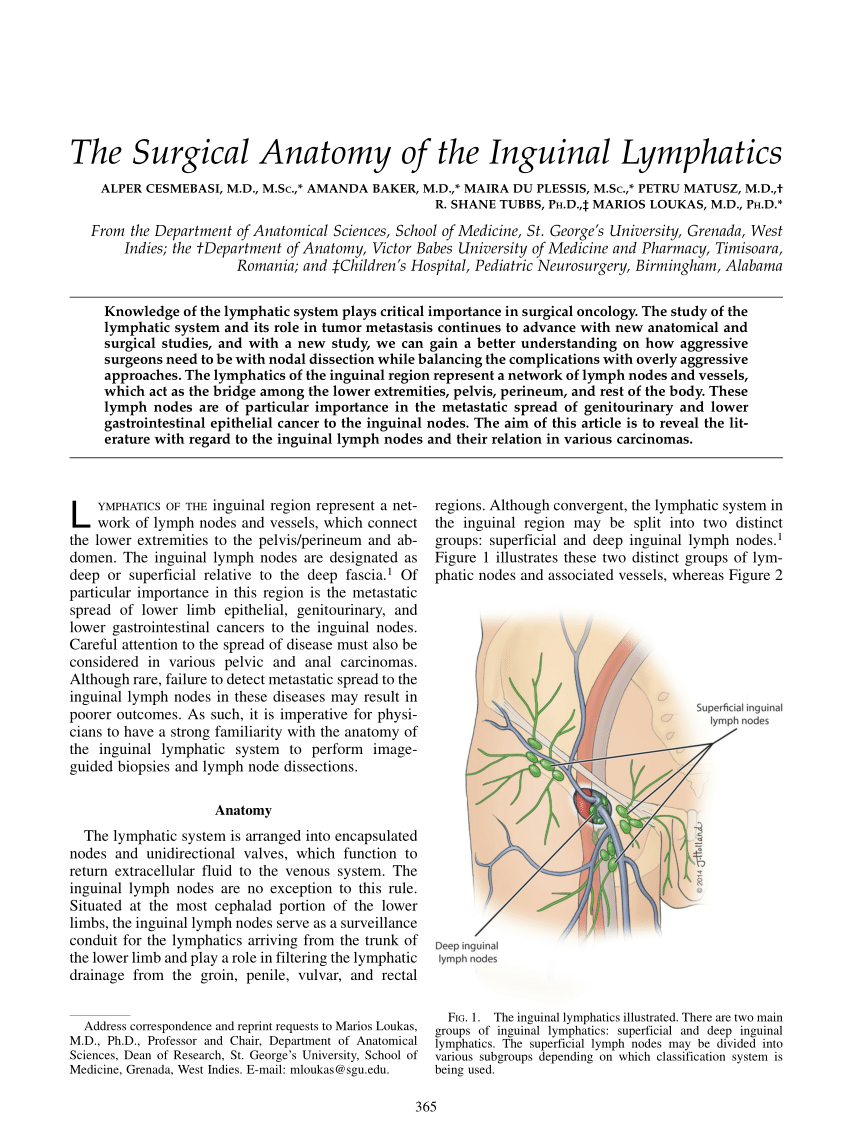
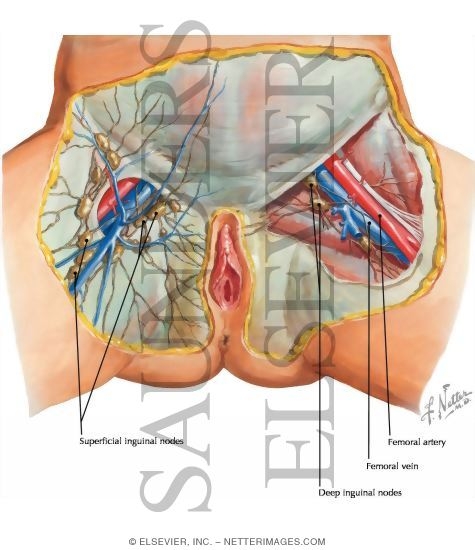
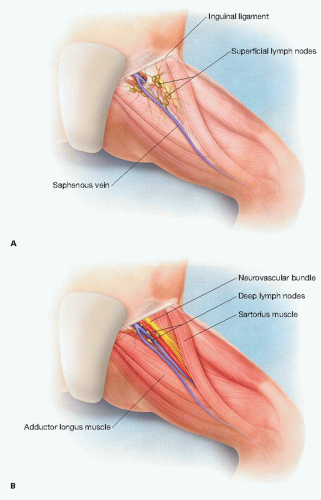
Swollen Lymph Nodes: Locations, Causes, Signs, Test & TreatmentWarning: The NCBI website requires JavaScript to operate. NCBI Bookshelf. Service of the National Library of Medicine, National Institutes of Health. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan... StatPearls [Internet]. Anatomy, Abdomen and Pelvis, Inguinal Lymph NodeToai Bui; Bruno Bordoni.AuthorsAfiliations Last Updated: February 7, 2021.Introduction Inguinal lymph node can be subdivided into the superficial and deep lymph nodes and collectively drain the anal canal (under the sinful line), the skin under the umbilicus The main function of the lymph node is to filter harmful substances as lymph fluids travel through their bark, paracortex and medulla. Clinical signs of inguinal lymphadenopathy can help doctors detect possible diagnoses of sexually transmitted diseases such as syphilis, chancroid, and venereum linfgranuloma. The lymph node can also help diagnose cancer. Structure and FunctionThe lymph nodes are small kidney-shaped rounded structures that work with the lymph system. Lymph nodes play a vital role in the body's ability to fight infection. A capsule of resistant fibrous connective tissue encapsulates the lymph nodes. The fibrous capsule extends to the lymph node to form trabecula and divide each node into lobes. The different size of lymph nodes has a different number of lobes. Each lobe is divided into separate compartments; bark, paracortex and medulla; the cortex houses the primary follicles, which are inactive B-cell lymphocytes. Paracortex hosts T-cell lymphocytes. Medulla contains reticular and macrophages cells and communicates with efferent lymph vessels. The lymph node has aferent vessels that carry lymph fluid to the lymph node. As the fluid travels through the lymph node, immune cells within the node filter for harmful substances such as bacteria, viruses, parasites and other foreign materials. If there is a presence of an antigen, the B-cell lymphocyte in the follicles creates antigen-specific antibodies. Activated primary follicles are formed in secondary follicles called germ centers and indicate the proliferation of B lymphocytes and the production of antibodies. Antibodies labeled the antigen for destruction by other immune cells. T-cell lymphocytes are responsible for immunity mediated by cellular cells. Macrofages fagocitin pathogens such as bacteria and viruses and destroy them. The lymph nodes are found throughout the body and can be found in deep and superficial tissues and drain specific areas of the body. Inguinal lymph nodes are in the area of the groin and classify as shallow and deep. Surface inguinal lymph nodes reside under the inguinal ligament and subdivid in the lower, superolateral and superomedial nodes. The superficial inguinal lymph nodes drain the anal canal (under the pectined line), the skin under the umbilicus, the lower extremity, scrotum and vulva. Deep inguinal lymph nodes are within the femoral mean of vain to the femoral vein. Deep nodes receive the drainage of the penis from the glans or clitoris, as well as the superficial lymph nodes. Surface and deep inguinal lymph nodes are drained into the external lymph nodes. Embryology The development of lymph nodes begins from 11 weeks of gestation as a mesenchymal condensation that gives rise to the lymph node capsule and connective tissue. The T-cell lymphatic region begins development during 13 weeks. The B-cell lymphatic region begins during 14 weeks. From week 13, monocytes and macrophages may be present with the lymphatic sac. During the 20 weeks, follicle, paracortex and medulla are discernible and continue to develop throughout the pregnancy and after birth. The lymphatic system is derived from the mesodérmic embryonic leaf. Blood supply and lymphaticArtery enters from the hilum, a depression on the concave side of the lymph node, on the concave side of the structure in kidney form. The artery passes through medulla and bark. Once in the bark, the branches of the artery in the arteries and capillaries. The vein comes out of the hilum lymph node as well. The aferent lymphatic vessel enters the lymph node on the convex side of the node. The afferent vessels carry lymph through one-way valves and the node where it is distributed through the breasts. After the lymphatic fluid is filtered, it exits through the efferent lymphatic vessels of the hilum. Efferent vessels also have one-way valves to prevent the flow of return of lymph fluids. Nerves The femoral nerve is in the Scarpa triangle or femoral triangle. Swollen lymph nodes can compress the nerve and cause femoral neuropathy. Surgical Considerations The inguinal lymph node resides within the femoral triangle. The femoral triangle is bound by the inguinal ligament, the aductor longus muscle and the sartorius muscle. The lata fascia forms the roof of the femoral triangle. The soil of the femoral triangle shape of the iliopsoas and the pectineus muscles. On the day of surgery, nano coloids of tecnetio-99m are injected into the primary site of cancer. The location of the sentinel node is found using a portable gamma camera. The blue dye is also often injected into the primary cancer site to help visualize the sentinel node after making the incision. Incision is performed parallel to the inguinal ligament, and the inguinal inguinal lymph node can be found medial to the femoral vein. A surgical approach in this area can give several adverse symptoms for the patient: Clinical MeaningLymphadenopathyLymphadenopathyInflamed lymph nodes usually indicate bacteria or virus infection. Inguinal swollen lymph nodes may indicate an infection of the lower body areas. One of the most related causes of inguinal lymphadenopathy is sexually transmitted infections. Sexually transmitted infections commonly occur with inguinal lymphadenopathy are the venereum of lymphogranuloma, secondary syphilis and chancroid caused by chromodia trachomatis (L1-L3), Treponema pallidum and Haemophilus ducreyi, respectively. Linfogranuloma venereumLymphogranuloma venereum is a genital area disease caused by the Chlamydia trachomatis gram-negative bacteria (L1, L2, and L3). The lymphatic venereum mainly affects the lymphatic system and has three stages. The secondary stage of the linfagranuloma venereum may be presented with tender unilateral or bilateral inguinal lymphadenopathy. SyphilisSyphilis is a bacterial infection caused by Treponema pallidum spirochete. The clinical presentation of the secondary syphilis can be presented with diffuse lymphadenopathy along with fever, skin rashes and condylomata lata. ChancroidChancroid is a rare sexually transmitted disease caused by a small gramnegative rod, Haemophilus ducreyi. 50% of infected individuals present with tender inguinal lymphadenopathy along with exudate ulcers.LymphedemaLymphedemaThe inflammation that typically occurs in the arm or leg due to lymph vessels that cannot drain the lymph fluid sufficiently. Inguinal lymph node damage may occur with lymphedema of the lower limb. Infection-related lymphedema is more common in developing countries in tropical and subtropical regions. Wuchereria bancrofti is a nematode known for causing leg lymphedema. Transmitted by mosquito bites, Wuchereria bancrofti invades lymph nodes and causes inflammation and damage to the lymph node and lymphatic system. In developed countries, the causes of lymphedema are commonly due to malignity or the treatment of malignancy. Treatment includes excision of malignant lymph nodes for diagnosis and treatment of radiation. Cancer Diagnosis Cancer Diagnosis Cancer Cancer cancer may appear in the lymph node as the primary site of the cancer or may spread there from another primary site. Cancer cells are able to migrate through the lymph system and end up in a lymph node that is draining the primary site. For carcinomas that are spread through the lymphatic system, they are commonly spread to the regional node before extending to the next node level. These immediate regional nodes are called sentinel lymph nodes. If the clinician suspects that an individual has cancer, a biopsy or sentinel lymph node dissection that is draining the site of interest can help determine whether the cancer has metastasized. By finding a cancerous cell in the sentinel lymph node, this information can help with cancer staging and direct therapy mode. Common tumors that metastasis in the inguinal lymph node include squamous vulva carcinoma, penis, and anus. Vulvar Cancer Vulvar is the area of the skin that surrounds the urethra and vagina. Vulvar cancer is more common in postmenopausal women and may occur with lumps or bumps and itching. Other symptoms include tenderness, bleeding, and skin changes. Precise etiology of vulvar cancer is unknown, but some factors increase the risk of someone having vulvar cancer. These risk factors include the older age, exposure of the human papillomavirus, smoking, a weakened immune system and a skin condition that involves vulva. Penis Cancer Penis cancer is most common in Asia, Africa, South America. Penis cancer begins as a small injury to glaciers that varies in appearance. The injury may appear as masses that grow from the skin or from the white or reddish mass. Risk factors include infection of the human and uncircumcised papillomavirus. Other risk factors include the history of phomosis, balanitis, chronic inflammation, tobacco use, lichen sclerosis and poor hygiene. Anal Cancer Kidney cancer is cancer that occurs in the anal canal. Patients may have anal bleeding, weight loss, mass sensation, tenderness and itching. Risk factors include the most advanced age and human papilloma virus infection. Other ProblemsDigeorge syndrome is due to a small elimination in chromosome 22, which leads to poor development in various organ systems. One of the problems commonly present in someone with DiGeorge is the dysfunction of the thymus gland. The thymus gland is where T cells mature and help combat infection; therefore, thymus gland dysfunction will result in T-cell deficiency. T-cell deficiency will result in paracortex of lymph nodes that are not well developed. Continuous education/review questions Limfatic System, cervical lymph nodes, lymphatic of the breast gland, chyli cisterna, lumbar lymph nodes, pelvic lymph nodes, lymphatic lymphatic lower extremity, chest duct, thymus, lymph nodes Axillary, spleen, upper lymphatic, extremity This book is distributed under the terms of the Creative Commons 4.0 International License ( Creative Commons 4.0), which allows the use, duplication, adaptation, distribution and reproduction in any medium or format, provided that you give appropriate credit to the original author(s) and source, a link to the Creative Commons license is provided, and changes are indicated. ViewsIn this PageRelated information Similar products in PubMed Recent activityYour navigation activity is empty. The activity recording is off. , 8600 Rockville Pike, Bethesda MD, 20894 USA

Department of Surgery - Lymphadenectomy

Inguinal lymph nodes - Wikiwand

Inguinal lymph nodes - Wikipedia

The Future of Inguinal Lymph Node Dissection Is Robotic – Consult QD

Lymph Nodes Picture Image on MedicineNet.com
Radiation Therapy to Your Lymph Nodes | Memorial Sloan Kettering Cancer Center

Nodes removed in inguinal versus ilioinguinal completion lymph node... | Download Scientific Diagram

The One Ovulation Sign You've Never Heard Of
![Figure, Lymphatic System, Cervical lymph nodes,...] - StatPearls - NCBI Bookshelf Figure, Lymphatic System, Cervical lymph nodes,...] - StatPearls - NCBI Bookshelf](https://www.ncbi.nlm.nih.gov/books/NBK513317/bin/lymphaticSystem.jpg)
Figure, Lymphatic System, Cervical lymph nodes,...] - StatPearls - NCBI Bookshelf

Inguinal lymph node - www.medicoapps.org
:background_color(FFFFFF):format(jpeg)/images/article/en/lymphatic-vessels-and-nodes-of-the-pelvis/XDRgznWy8xClzjk2n9HmAA_qDiCg56SIU92Uj9OWe79A_Common_iliac_lymph_nodes_02.png)
Anatomy of the pelvic lymph nodes and vessels | Kenhub
Inguinal lymph nodes

Anatomical zones in inguinal node dissection. | Download Scientific Diagram

Pelvic Lymph Nodes | NorthShore
Lymph node removal (lymphadenectomy) | Health Information | Bupa UK

Deep inguinal lymph nodes - Wikipedia, the free encyclopedia | Lymph nodes, Lymph massage, Lymphatic system
What happens when cancer spreads to the lymph nodes? - Macmillan Cancer Support

Orchid | Lymph Node Dissection
Imaging of Pelvic Lymph Nodes | SpringerLink
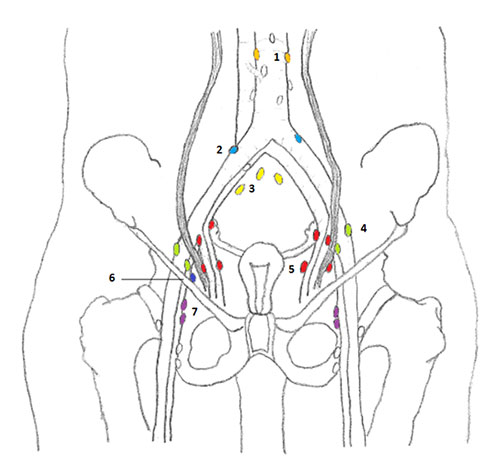
SEER Training: Lymph Nodes of Female Pelvis

Endoscopic Subcutaneous Modified Inguinal Lymph Node Dissection for Squamous Cell Carcinoma of the Penis | Abdominal Key
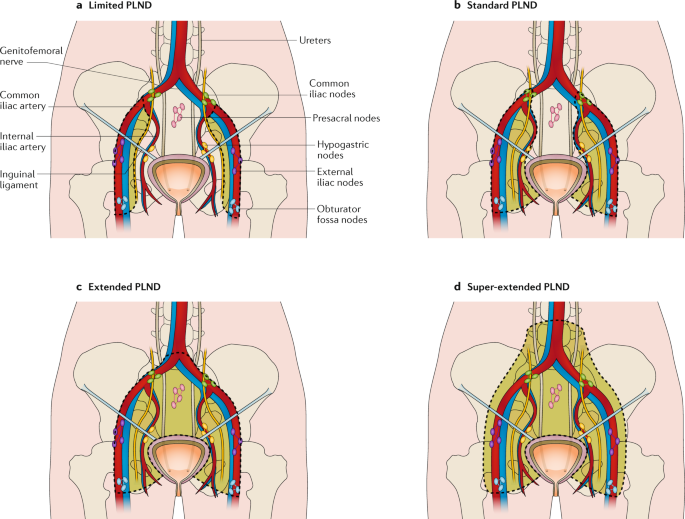
Pelvic lymph node dissection during radical cystectomy for muscle-invasive bladder cancer | Nature Reviews Urology

Lymphatic Drainage of Lower Limb , Anatomy QA
:background_color(FFFFFF):format(jpeg)/images/library/2335/nQ9zLwvCpLezSf5dQRG32Q_Nll._inguinales_superficiales_02.png)
Lymph nodes of the pelvis and lower limb: Anatomy | Kenhub

A New, More Convenient Way to Treat Allergies

Inguinal (Groin) Lymph Nodes - thelymphnodes.com | Lymph nodes, Lymph node massage, Lymph massage

Deep Inguinal Lymph Nodes - an overview | ScienceDirect Topics
%20with%20labels.jpg)
British Association of Dermatologists - Patient Information Leaflets (PILs)
Where are your lymph nodes? - Quora
How to check your lymph nodes | Skin Support

The Future of Inguinal Lymph Node Dissection Is Robotic – Consult QD

Unexplained Lymphadenopathy: Evaluation and Differential Diagnosis - American Family Physician
Lymph nodes in the female lower abdomen and pelvis - Macmillan Cancer Support

Common Iliac Lymph Nodes - an overview | ScienceDirect Topics
PDF) The Surgical Anatomy of the Inguinal Lymphatics
Inguinal Lymph Nodes
Surgical Technique for Open Inguinal Lymphadenectomy | SpringerLink

AUA 2019 Annual Meeting
Minimally Invasive Inguinal Lymph Node Dissection for Melanoma | Basicmedical Key
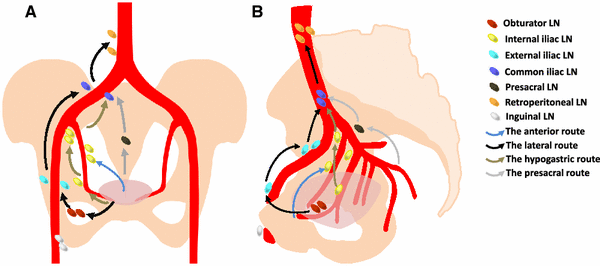
Does Lateral Pelvic Lymph node matters in rectal cancer
Posting Komentar untuk "inguinal lymph nodes location"